Regional Transfer & Referral Centers
HMR, LLC on Regional Referral Programs
Growing Census Through Regional Referral Programs
A regional referral center is a hospital or health system that is established to support a high volume of transferred patients in the region with complex Medical, Surgical and Trauma cases. A state-of-the-art Regional Referral Center employs a centralized Transfer Center, which functions as a one step service that coordinates transfers if a patient needs additional complex specialty care.
Transfer Center Development
- A Transfer Center is a highly efficient, centralized resource for physicians and medical facility staff to coordinate patient flow within a health system, or between health system facilities and non-affiliated providers or hospitals. With a single phone call or electronic activation, the Transfer Center process manages all aspects of patient movement, including: physician consultations, bed coordination, chronological documentation and records distribution, communication between referring and receiving physicians/facilities, arrangement of transport, and all other system-specific needs related to comprehensive patient movement. Three primary goals of any successful Transfer Center program should be (a) the efficient and timely coordination of appropriate patient care, (b) providing the hospital or health system with the ability to manage patient flow in a manner that supports organizational strategy and (c) position the ACO for Population Management with a Patient Concierge Service.
- With a state of the art Transfer ‘One Call’ Center, the return on investment is typically 15:1.
HMR conducts an evaluation of the volume of potential referrals, determines the readiness of the Medical Staff specialty panels to accept new referrals and assists with the design and implementation of the new Transfer Center to achieve best results.
Healthcare Consumers
Healthcare consumers have more choices now than ever before. In response, employer groups are demanding more tools and better strategies to drive wellness program engagement. At the same time, impacts of the Affordable Care Act (ACA) mean health plans are competing more directly for consumers in an increasingly transparent marketplace. With the Accountable Care Organization, the transition from Fee For Service to Fee for Value will continue to escalate, especially in competitive environments.
Patient Engagement
A member engagement framework can help the Medical Center map out a plan for attracting consumers to your wellness tools, either directly or through their employers. And it’s the structure that lets an ACO build on their individual successes to keep patients engaged, healthy, satisfied, and loyal—year after year.
The six key elements that create a framework for member engagement and loyalty are:
- Access,
- Appeal,
- Outreach,
- Rewards,
- Brand, and
- Feedback.
Each Medical Center will need to build its own member engagement framework so the ACO can successfully acquire and retain members, and the affiliated employer groups meet their population wellness goals.
Importance of Post-Acute Continuum
Post-acute services continue to drive substantial cost variations for organizations looking to manage avoidable spending. Although providers must build a comprehensive network, partnering with and managing the transition to post-acute care must be a key care redesign initiative in 2015. Losses along your referral pathways are preventable and can yield impressive returns.
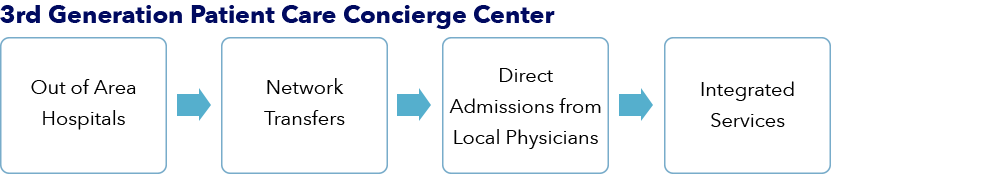
Developing the 3rd Generation Patient Care Concierge Center
Left unmanaged, cracks develop in the referral pathways which can weaken your network and allow funneling of patients out at an alarming rate. More often than not, the physician’s front office staff determines whether a referral stays in network or leaks to your competition—a decision made based on ease and convenience.
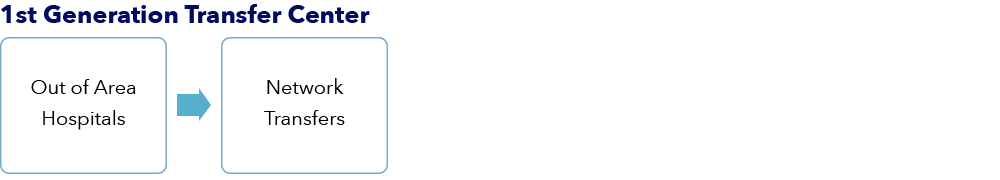
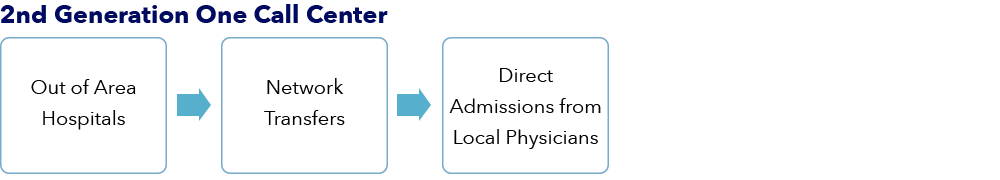
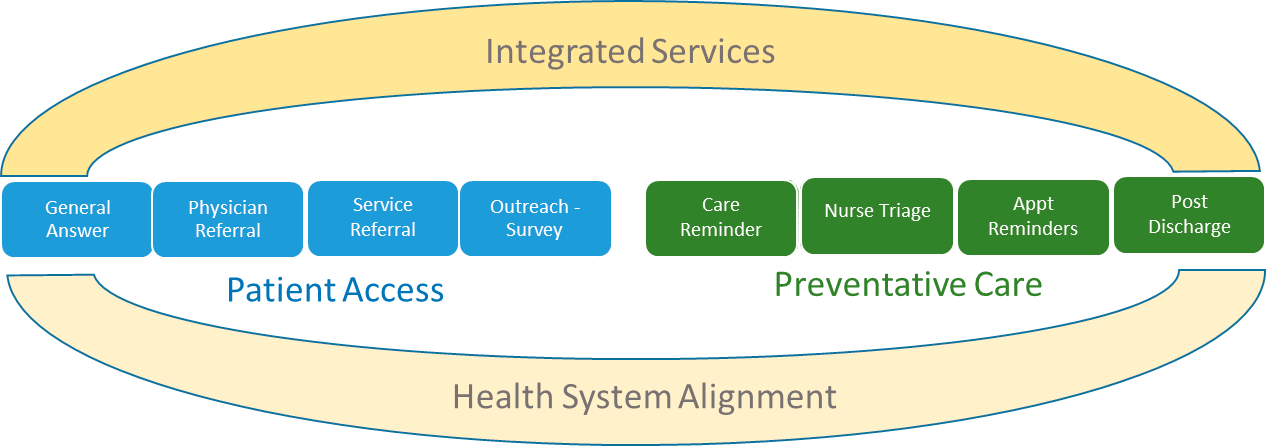
The first generation ‘Transfer Centers’ focused on marketing specialists to smaller hospitals needing a higher level of care. The second generation ‘One Call Centers’ added the ability for the local physician community to easily admit patients directly to a bed, avoiding the costly and time-delayed experience through the Emergency Department. The third generation ‘Patient Care Concierge Center’ provides all of the services to accept out of area transfers, ease of referral from the local community physicians and adds a new component, ‘integrated services’. This includes a call center that adds Home Interactive Devices, Advice Lines and Post Discharge Follow Up. Organizations utilizing referral-matching technology and online scheduling take the upper hand. With a centralized, coordinated and efficient Patient Concierge Center in place, the ACO would be positioned well to leverage its operations to further navigate through population health management and better manage at-risk patients.
Trademark: HMR, LLC
Call Center
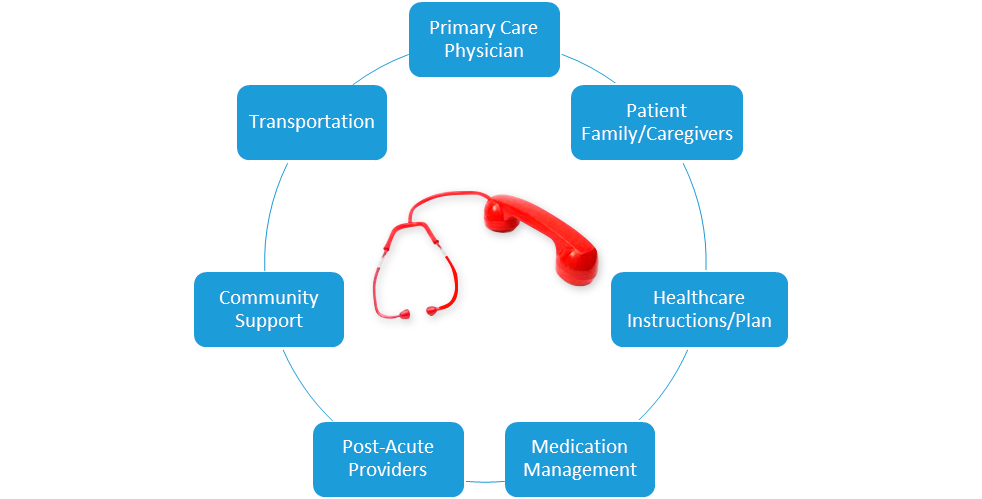
A call center that manages acute transfers and direct admission can also be utilized for other “Integrated Services”. These services are meant to help navigate (and control) patient interactions and care, outside of the acute care setting.
- Home Interactive Device – Sophisticated health systems are finding creative ways to better brand themselves in competitive markets, identify risk and better align patients with a provider, facility, or system. A successful way to achieve these goals is to implement a Home Interactive Device. This device is a simple communication hub that is placed in a patient’s home and connects a patient to the health system. The patient accesses healthcare communication through the device, both emergent and non-emergent. Communication to the patient occurs through the device and allows the patient to have immediate access to care (reactive and proactive), anytime, in their home.
- Healthcare branding – The device itself is branded with the health system logo and when the patient accesses communication through the device, the call center representative identifies themselves as the health system, ensuring appropriate care and response.
- Patient alignment – Through the device, patients align themselves with a health system and identify care through the device. Patients can be triaged and sent to the most appropriate and cost effective care solution for their needs.
- Concierge services – Access to other medical related needs can be coordinated with access to the call center. Medication refills, DME and delivery, primary care appointments and non-emergency transportation are all sample services that are coordinated by this service.
- Advice Line Services/Nurse Triage – A call center staffed with RNs can be utilized as a simple advice line service to managed care patients. This service can be a value- add advice line for a care plan, or as a nurse triage to ensure proper access to care in the event of acute care needs (urgent care, clinic, ED). This work is non-emergent and can often be done “on the margin” in the call center, increasing productivity of call center staff.
- Post Discharge Follow Up – Post acute care patient follow up increases patient satisfaction (pre-HCAHPS survey) and provides the necessary linkage to post-acute care to reduce readmissions. Implementing a post discharge call program through the call center is a simple way to provide this service to a health systems patients. Metrics should be identified and results tracked. Successful programs include monitoring of key performance indicators such as; percentage of patients who understood discharge instructions by hospital unit, percentage of patients who have successfully reconciled their medications and percentage who have followed up with primary care.
- Discharge instructions – By accessing EHR, the call center staff can quickly asses a patients understanding and compliance with discharge instructions. Outliers, or triggers can be managed to Case Management, or to a patient RN navigator for in depth follow up and follow through.
- Medication Reconciliation – Medication compliance failures are the most common cause of readmission following an acute care stay. Patients often do not follow the needed steps to ensure medication lists are sent to their pharmacy, or primary care. The call center can access these records, provide an overview to the patient and ensure prescriptions are sent to the correct pharmacy, even arranging delivery, if needed.
- Primary Care Communication and Follow up – The most common feedback from primary care providers, following an acute care admission, is that there is a lack of communication back to primary care. Patients fail to do this on their own and hospitals are often not structured to have this process in place. The call center, through its follow up process, can facilitate the delivery of acute care admission information back to primary care and can also be the vital linkage with patients to ensure primary care follow up appointments are made and kept.
- Physician Referral for ED Unassigned Patients – Equally important, engaging the patient following a hospital discharge allows for the opportunity to align non-assigned patients with a health system medical group. This can be accomplished through intelligent workflow, ease of system integrations and the call script itself. Patients who do not have a primary care, or specialist assigned can be efficiently managed into a preferred group, on the merits of customer service and quality post-acute care.
Only a few Health Systems in the US are mature enough to appreciate the opportunity to implement a 3rd Generation Patient Care Concierge Service. HMR would determine if your Medical Center and ACO are positioned to provide this type of service. The recommended approach is to partner with an expert who can expedite the implementation and allow focused attention to developing the latest generation model.